Case Report
Year: 2022 |Volume: 1 | Issue: 03 |Pages: 158-163
A CASE REPORT: EXTRACTION OF MIGRATORY FOREIGN BODY (SHALYA NIRHARANA)
About Author
Correspondence Address:
: Dr. Kamlakar Prakash Shahare, PG Scholar, Department of Shalyatantra, Shri Ayurved Mahavidyalaya, Nagpur, Maharashtra, India, Mob no. 9765654042, 9529161313, Email-kamlakar508@gmail.com
Date of Acceptance: 2022-09-30
Date of Publication:2022-10-16
Article-ID:AYU_29_10_22 https://ayuscript.com
Source of Support: Nill
Conflict of Interest: Nill
How To Cite This Article: Shahare KP, Shinde J, Badwe Y, Rangari AR, A Case Report: Extraction Of Migratory Foreign Body (Shalya Nirharana). AYUSCRIPT 2022;1(3):75-78
Abstract
Introduction - Acharya Sushrut defined Shalya Tantra as the science that deals with the removal of different kinds of Shalya (foreign body) and application of Yantra, Shastra, Kshara, Agni and Vrana Nidana. Acharya had given separate chapter for Pranashta Shalya (foreign body) Diagnosis and its removal. Acharya Sushrutha considered, that which is causing pain to body as “Shalya”. Pranashta means that which is not visible. Pranashta Shalya means invisible foreign body hidden inside the body. Foreign body ingestion and impaction remains a common problem both in paediatric and adult populations.
Method – A 14 years old male patient having history of ingestion of fish bone 1 yr ago for this he took home remedies and treatment at private hospital. X-ray s/o of no any abnormalities but patient got no relief after 6 month of ingestion, abscess formed and burst externally and there was pus discharge (on and off) from small opening near hyoid bone anterior aspect of neck on the left side since 6 months. Patient was planned for exploration and extraction of foreign body under general anesthesia which is the necessary and immediate treatment. In this case study urgent exploration and extraction of foreign body was done to prevent irreversible sequelae, as foreign body that is not quickly extracted and they can cause several life-threatening complications such as perforation of the esophagus, deep neck infection/abscess, mediastinitis / mediastinal abscess, and aortoesophageal fistula.
Result- Patient recovered from pain completely after removal of foreign body and disappear hyper echoic area Ultra sonographycally. No any complication / discharge noted upto 6 months after surgery.
Conclusion- In this case an effort has been made to draw special attention on ancient surgical concepts of Sushruta Samhita practicing today with few refinement. Penetrating wounds can damage nerves or blood vessels. Evaluating patient’s sensation and circulation is essential. Superficial foreign bodies can sometimes be palpated or visualized. Deeper foreign bodies may require additional methods to localize.
Keywords- Pranshtashalya; Shalya Nirharana; Fish Bone; Foreign Body; Migrating Foreign Body.
Introduction
Acharya Sushruta considered, that which is causing pain to body as “Shalya”(1). Pranashta means that which is not visible. Pranashta Shalya means invisible foreign body hidden inside the body(2). Pranashtashalyaadhyaya(3) is an exquisite piece of work titled by Acharya Suhsruta, which entails about the different dimensions of the Ayurveda science. Acharya Sushruta has mentioned eight types of surgical procedures to fulfil the aim of Ayurveda of Dhatusamyata through Shalyatantra entity(4). Ashtvidha shastra karma- Eight kinds of surgical techniques(5,6,7 are to cure tissue injury and inflammatory conditions. They are Chedana (Excision, amputation, resection), Bhedana (incision, counter incision), Lekhana (scrapping, scooping), Vedhana (Puncturing, penetration), Eshana (Probing), Aharana (extraction and removal), Vistravana (Evacuation, Emptying, drainage) and Seevana (Suturing, Ligation). Foreign body ingestion and impaction remains a common problem both in paediatric and adult populations. In children, the highest incidence of impaction typically occurs between the age of 6 months to 3 years, and the most common ingested foreign bodies include coins, small toys, button batteries and magnets(8). Compared to adults, children in Western populations rarely ingest fish bones. However, previous literature has demonstrated that in countries with a higher fish intake, such as those in Asia, there is an increased incidence of fish bone ingestion and impaction in both children and adults(9).
Fish bone ingestion possess significant potential hazards regardless of age, including visceral gastrointestinal perforation, secondary deep neck abscesses or mediastinitis and delayed oesophageal stenosis(10). Therefore, regardless of the demographics, fish bone ingestion necessitates accurate diagnosis and appropriate evidence-based management. Pediatric fish bone ingestion presents its own unique challenges. Paediatric fish bone ingestion may provide a diagnostic challenge as a result of difficulties obtained with history-taking from the child, the event frequently unwitnessed by the carers and identification of the exact location of the bone. Although the size of the foreign body has not specifically been assessed in fish bone impactions, it is a well-established predictor for impaction risk in other foreign bodies such as coins(11,12).
Although fish-bone foreign bodies are not frequently associated with severe complications, they can cause several life-threatening complications such as perforation of the esophagus, deep neck infection/abscess, mediastinitis/mediastinal abscess, and aortoesophageal fistula(13,14,15).
Case report: 14 year old Male patient was brought to the surgery OPD of Pakwasa hospital having history of ingestion of fish bone 1 year Ago for this he took home remedies and treatment at private hospital but still had mild pain and difficult during deglutination. X-ray s/o of no any abnormalities but patient got no relief. After 6 months of ingestion, abscess has been formed and had burst externally and there was pus discharge (on and off) from small opening near hyoid bone at anterior aspect of neck on the left side since 6 months. The discharge was more after taking meal .On local examination, there was small (0.5 X 0.5cm) opening in the lower part of the neck of left side hyoid bone. Some pus discharge was found on pressing near its external opening. X-ray spine and cervical (AP): (24/02/2021) revealed no any significant abnormality. USG REPORT :( 20/02/2021) showed Chronic Hematoma secondary to linear foreign body in neck. CT NECK (plain & contrast) reports revealed: (20/09/2021) Focal small peripherally enhancing hypodense lesion with linear hyper density in middle seen in right infrahyoid region level III .There is small external opening noted – likely abscess with foreign body. Linear abnormal t-2 hyper intense sinus track seen extending superiorly from left parasagittal supraclavicular skin surface to deeper tissue of neck ends blindly in submandibular region. No evidence of any cyst or abscess in underlying soft tissue. ? branchial sinus/fistula. Patient was planned for exploration and extraction of foreign body under general anaesthesia. Under AAP under GA patient in Supine position parts painted, drapped and isolated. .Transverse elliptical incision taken including external opening of sinus .Incision deepened up to platysma muscle. Fibrous tract was dissected .It was adherent to external Carotid vein which had bleed while dissection. And Rent with prolene (2-0) .Another transverse incision taken superiorly and deepened up to tract. Tract was opened and foreign body removed .Scooping done and sinus cavity closed with vicryl 2-0. Skin Closure done with Vicryl 2-0 (Simple interrupted sutures) .Packed well. Dressing done. All procedure was uneventful. Excised tissues were sent for histopathological examination of tissue. Histopathology confirmed tract lined by chronic inflammation and removed foreign body (fish bone) with confirmation of foreign body (fish bone) obstruction with wound at anterior aspect of neck as final diagnosis. Sutures removed after 10 days. Periodic follow up were taken upto 3 months to rule out any recurrences.
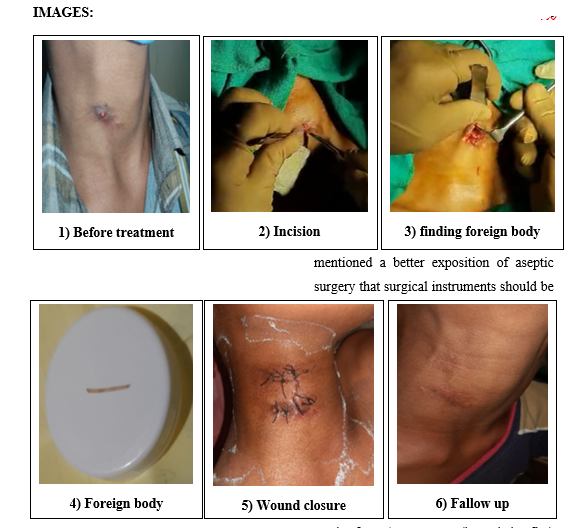
img
Discussion
Patient recovered from pain completely after removal of foreign body and there was disappearance of hyper echoic area Ultra sonographically. Penetrating wounds can damage nerves or blood vessels. Evaluating patient sensation and circulation is essential. Superficial foreign bodies can sometimes be palpated or visualized. Deeper foreign bodies may require additional methods to localize. Sushruta and his commentator Dalhan mentioned a better exposition of aseptic surgery that surgical instruments should be used after Agnitaptena (heated in fire) otherwise risk of suppuration may happen(16). Sushruta made attention about ideal quality of incision, correct technique of incision, correct shape of incision at particular site, direction of incision, extension of incision, method of suturing, complication of improper incision etc. Sushruta advises the careful haemostasis during any kind of surgical procedure. After incision in surgical procedure or removal of foreign body make sure Nirlohitam vranam kritwa (make blood leakage free) by appropriate measures(17)
Conclusion
In this case an effort has been made to draw a special attention on ancient surgical concepts of Sushruta Samhita practicing today with few refinement. In this present case study, a foreign body in the form of fish bone was successfully excised. A surgeon should come to accurate diagnosis clinically and investigate thoroughly and then plan for the excision of foreign body with all aseptic precautions as soon as possible before it leads to any secondary complications.
Consent of patient: The written consent has been taken from relatives before the procedure as well as to publish the case report without exploring identity of the patient.
References
- Acharya Sushrutha, Sushrutha Samhitha, English Translation, Translator Prof. K. R. Srikantha Murthy, Chaukhambha Publishers, Edition, Vol1, Suthrasthana, 2012; 26/5: 189-239.
- Acharya Sushrutha, Sushrutha Samhitha, English Translation, Translator Prof. K. R. Srikantha Murthy, Chaukhambha Publishers, Edition, Vol 1, Suthrasthana, 2012; 26/5: 189-239.
- Susruta, SusrutaSamhita with NibandhaSamgraha and Nyayachandrika commentaries, Ed. Vd. Y.T Acharya, Chaukhambha Orientalia, Varanasi, 2009 (Reprint), Sutra Sthana.26: p.121.
- Pro G D Singhal & Colleagues Sushruta Samhita, (English Translation) Part 1 Sutra Sthan, 5/ Agropaharaniya adhyayah, 5 Chaukhambha Sanskrit Pratishthan, Varanasi. 2007; p-44.
- Susruta, Susruta Samhita Vol. I (Edited with Ayurveda Tattva Sandipika) by Kaviraj Ambika dutta Edition Print 2010, Chaukhamba Sanskrit Sansthan. Sutra sthana 5/5.
- Charaka, Charaka Samhita Vol. II (Edited with Vidyotini Hindivyakhyyopeta) by Pandit Kashinath shastri and Dr. Gorakhnath Chaturvedi Edition print 2012, Chaukhamba Bharti Academy. Chikitsa sthana 28/5.
- Vagbhata, Ashtang hridyam Edited with Nirmala Hindi commentaryby Dr. Brahmanand Tripathi, chaukhamba Sanskrit Pratishthan, Varanasi, First edition 2001. Sutra sthana26/28,29.
- Dereci S, Koca T, Serdaro?lu F, et al. Foreign body ingestion in children. Turk Pediatri Ars 2015;50:234-40. [Crossref] [PubMed].
- Nandi P, Ong GB. Foreign body in the oesophagus: review of 2394 cases. Br J Surg 1978; 65:5-9. [Crossref] [PubMed].
- Ngan JH, Fok PJ, Lai EC, et al. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 1990;211:459-62. [Crossref] [PubMed].
- Singh N, Chong J, Ho J, et al. Predictive factors associated with spontaneous passage of coins: A ten-year analysis of paediatric coin ingestion in Australia. Int J Pediatr Otorhinolaryngol 2018;113:266-71. [Crossref] [PubMed]
- Reilly JS, Walter MA, Beste D, et al. Size/shape analysis of aerodigestive foreign bodies in children: a multi-institutional study. Am J Otolaryngol 1995;16:190-3. [Crossref] [PubMed].
- Kim HU. Oroesophageal Fish Bone Foreign Body. Clin Endosc. 2016;49(4):318–26. Epub 2016/07/28. pmid:27461891; PubMed Central PMCID: PMC4977739.
- Klein A, Ovnat-Tamir S, Marom T, Gluck O, Rabinovics N, Shemesh S. Fish Bone Foreign Body: The Role of Imaging. Int Arch Otorhinolaryngol. 2019;23(1):110–5. Epub 2019/01/17. pmid:30647794; PubMed Central PMCID: PMC6331292.
- Jha SK, Kumar SP, Somu L, Ravikumar A. Missing fish bone: case report and literature review. Am J Otolaryngol. 2012;33(5):623–6. Epub 2012/03/01. pmid:22365390.
- Shastri A, Hindi commentator of Sushrut Samhita, chikitsa sthan, Sadyovrana cikitsitam, 46, reprint ed. Chaukhambha Sanskrit Sansthan Varanasi, 2005 p.17.
- Shastri A, Hindi commentator Sushruta Samhita, sutrasthana, Shalyapanayaniya adhyayah, 27/8 reprint ed. Chaukhambha Sanskrit Sansthan Varanasi; 2005, p.111.
